The Sickening of America
Seventh and final part of the US economy series shows how the healthcare system is making us sick and emptying our wallets
Don’t miss Part 1: Introduction
Part 2: Legacy of the Great Recession
Part 4: Welcome to the New Gilded Age (monopolies)
Part 5: American Aristocracy (higher education)
Part 6: The Plague Economy (COVID-19)
Tl;dr
· The US spends more on healthcare but gets worse outcomes than its rich country peers
· Lifespans in the US have decreased, something not seen in the rest of the developed world
· Healthcare quality is split along class lines
· The US healthcare system is a collection of industry players with complex interactions but collectively does not optimize for patient health and wellness
· This failing system results in declining rural health, a rising epidemic of deaths of despair, a sick labor force, and declining US competitiveness
Healthcare has long been a major topic in American life. US President LBJ’s Great Society program rolled out Medicare and Medicaid – government sponsored health insurance – in the mid-1960s. More recently, President Obama expanded health insurance coverage with the Affordable Care Act (a.k.a. Obamacare) in 2010. Yet despite attention, the US healthcare system performs more poorly than its developed country peers.
The US spends $4 trillion (20% of GDP) on healthcare – 3x its developed country peers – but has health outcomes that came in last among 11 high-income countries in a 2021 report.[i]
The top-performing countries overall are Norway, the Netherlands, and Australia. The United States ranks last overall, despite spending far more of its gross domestic product on health care. The U.S. ranks last on access to care, administrative efficiency, equity, and health care outcomes, but second on measures of care process.[ii]
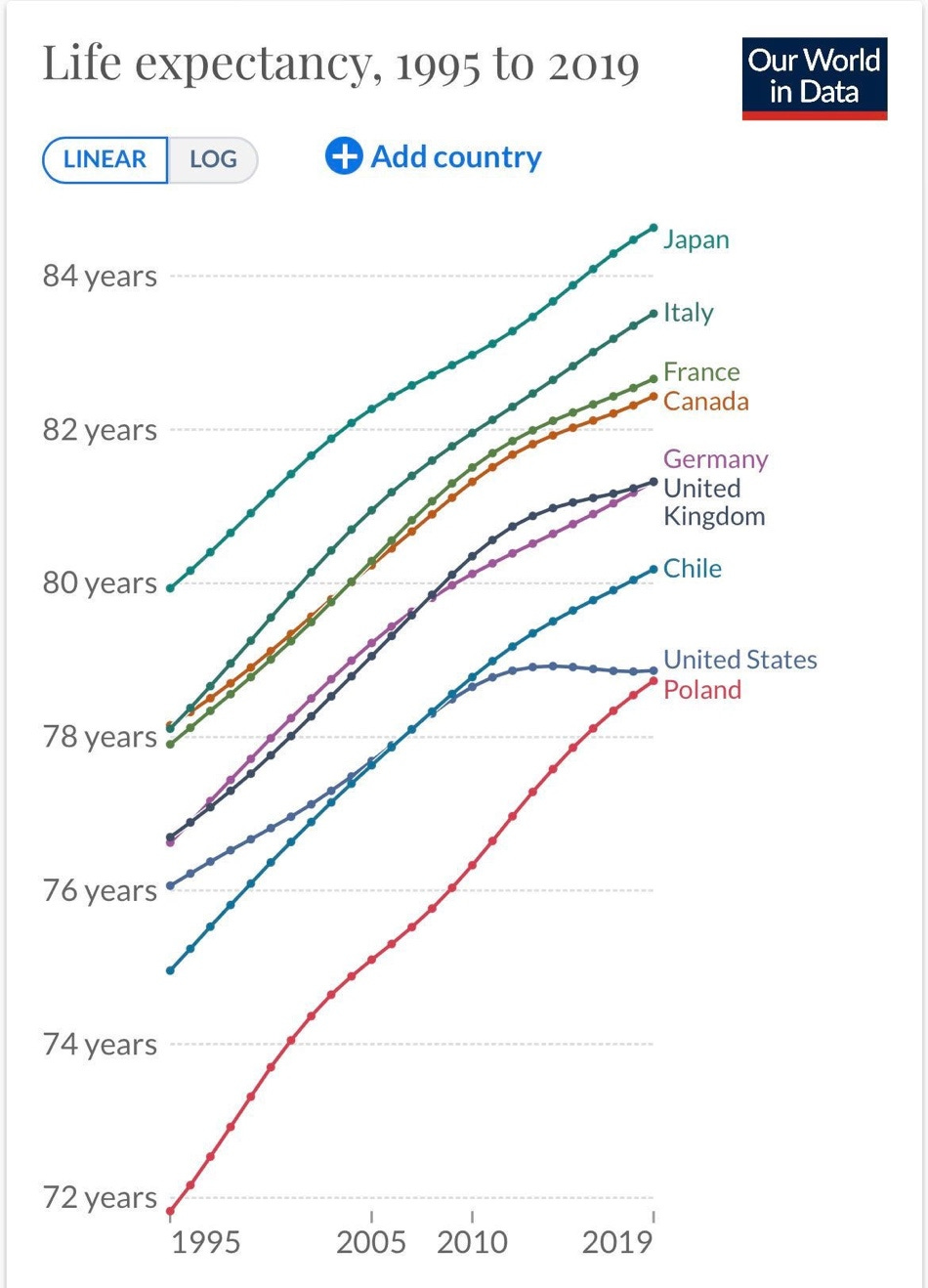
The US even does worse than developing countries on some measures. A shocking report from the World Health Organization in 2018 showed that lifespans in China had exceeded those in the US.[iii] In fact, a look at US lifespan data shows that lifespans have been stagnating since the mid-2000s in a way that isn’t occurring in other rich countries. Lifespans have even decreased some in recent years. So what has gone wrong in the US?
Figure 1: Falling US lifespans[iv]
Two Systems
A core feature of the US healthcare system is a theme repeatedly seen in Ad Astra’s US Economy series: a growing divide between the rich and the poor. The wealthy in the US – and those from all over the world – enjoy access to the best healthcare on the planet in America. This is true for almost all medical specialties. But the poor have access to worse care and have worse health outcomes. This brings the average level of care down and is why US fares poorly in global healthcare rankings. The relationship between income and inequality in health is obvious when life expectancy is overlain on a map of the US. Figure 2 shows that people in rich places like NYC and LA live longer than people in poorer places like the Midwest and Rust Belt.
Figure 2: Lifespans across the US[v]
Healthcare Industry Players
Any analysis of healthcare in the US must include an analysis of the healthcare industry. A rigorous evaluation of the healthcare industry could fill an entire book (such as Redefining Health Care by Michael Porter), but at a high level the US system is a collection of industry players with complex interactions who all serve different functions but collectively do not optimize for patient health and wellness. The partially-public nature of the system offers neither the innovative benefits of a fully private system nor the comprehensive coverage of a nationalized system. The main players in the system are as follows:
Primary Care
These are your primary care physicians and consolidated healthcare systems where you go for annual physicals and routine care. Historically practices were owned by physicians, but corporate urgent care providers (like national chains owned by CVS and Walgreens) are growing rapidly. Telehealth is a new service and can be used for some aspects of care, but much still requires an in-person visit to a bricks-and-mortar clinic. Primary care can be for-profit or not-for-profit.
Hospitals
Hospitals house Emergency Rooms (ER), the intake for any health emergency in the US. Calling 911 will deliver patients to the ER. You can also walk-in to any ER in America and get very expensive urgent care. US law requires that all patients, regardless of ability to pay, be treated in the ER.[vi] For-profit financial actors, such as private equity, are increasingly buying ER services. After a patient is stabilized, they may stay in a longer-term hospital ward. Hospitals also contain specialty departments like radiology, neurology, or cardiology. These specialize in a particular medical function. Hospitals can be for-profit or not-for-profit.
Specialty Outpatient Clinics
There are a wide variety of specialty outpatient clinics. Examples include dermatology, rehabilitation, imaging, dialysis, and many others. Outpatient means that a patient does not stay the night after a procedure. Patients are typically referred to specialty outpatient clinics by their primary care physician or the hospital. Specialty outpatient clinics can be for-profit or not-for-profit.
Pharmaceutical Industrial Complex
Any medications administered to humans originate from a complex, large industry that is best characterized as the Pharmaceutical Industrial Complex (PIC). Drugs originate from for-profit pharmaceutical firms, which can be small or large (e.g. Pfizer and Ely Lilly). These firms often develop drugs based on their profit-making potential. Physicians prescribe drugs to patients. Pharmacies (e.g. Walgreens and CVS) distribute drugs to patients. The media air advertisements (paid for by pharmaceutical firms) to viewers. The US is one of only two nations on earth that allows pharmaceutical advertising to the public (the other is New Zealand).[vii] In fact, a Harvard study found that the drugs with the highest advertising budgets typically have “low therapeutic value”.[viii] The Food and Drug Administration (FDA) is the government agency responsible for regulating the safety and efficacy of drugs in the US. FDA officials are often former or will soon be pharmaceutical firm employees, leading some to accuse the FDA of regulatory capture by the pharmaceutical industry. The PIC is almost entirely for-profit.
Insurance
At the center of this system are insurance firms, which reimburse healthcare providers (primary-care physicians, hospitals, specialty outpatient clinics, pharmacies) for their services. Pharmacy Benefit Managers (PBMs) are middle-man firms that can add significant cost to medications. Private insurers offer a wide variety of plans to consumers, which are paid for by periodic premiums by consumers or employers regardless of use. Public insurance is also offered by the government to retirees or low-income individuals, funded by tax revenue. Incentives created by insurers may influence upstream care and are not always aligned with the best care.
Taken together, this collection of players is the octopus that is the US healthcare system. This system is broken. The consequences of that failure have impacts across society.
Consequence 1: Declining Rural Health
Hospitals have closed in rural areas for the same reason airlines have cut flights to smaller cities: the low population density in rural areas cannot support most hospitals for-profit business models. Additionally, rural hospital have trouble finding young doctors and nurses to staff their facilities due to rural “brain drain”. The result is poorer care that makes these locations less desirable, harms labor markets, decreases economic development potential, and widens the growing rural-urban divide in America.
Figure 3: Rural hospital closures[ix]
Consequence 2: Deaths of Despair
In Part 3: Deindustrialization we saw how when jobs leave town, there is a downward spiral that leads to community collapse. Deindustrialization is a major cause of the growing epidemic of Deaths of Despair (suicides, alcohol-related, or overdose deaths). But the other cause is our failing healthcare system. Suicides can be prevented with more proactive mental healthcare, but our reactive healthcare system isn’t very good at promoting preventative wellness and many insurers don’t cover mental health care. The same can be said about alcohol treatment. The over-prescription of opioids and perverse incentivizes in the PIC fuel drug overdose deaths.[x] The result has been the doubling of Deaths of Despair in the US since the turn of the millennium. This trend has accelerated in recent years, with more than 700,000 drug overdose deaths from 2018-2022, many of them fentanyl-related[xi].
Figure 4: Suicides, alcohol-related, and overdose deaths[xii]
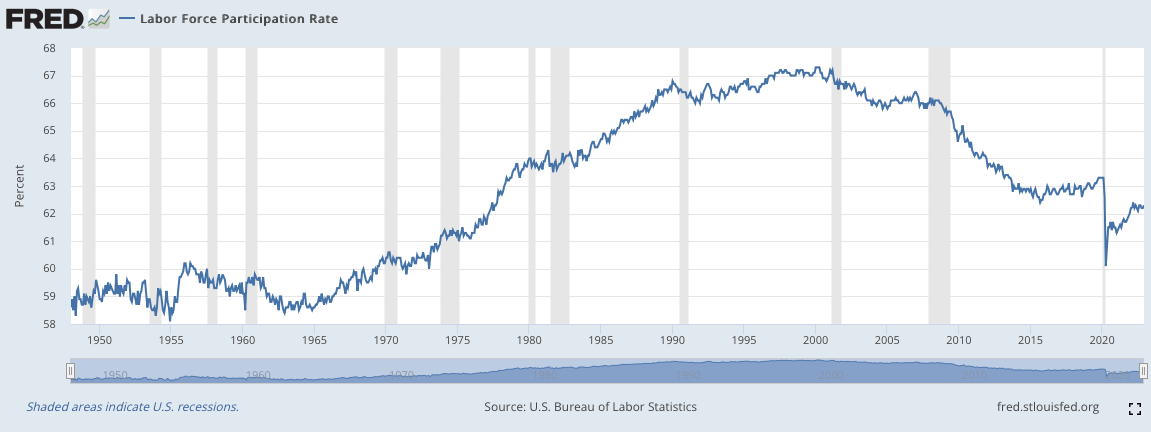
Consequence 3: A Sick Labor Force
The unemployment rate is widely reported by the media and currently sits at the low level of 3.4%, the lowest in 53 years[xiii]. In fact, there is a labor shortage – businesses can’t find enough workers. But the unemployment rate is a bad metric to describe America’s labor force. It only includes those who are actively looking for work and excludes those permanently sitting on the sidelines. A better metric is the labor force participation rate (LFPR), which includes the total US population. The LFPR has been falling since about 2000. If the US had the same LFPR as in 2000, 15 million more workers would be in the labor market; no labor shortage. There are many reasons why the LFPR is lower today than in 2000 but one reason is the increased number of people who aren’t working due to chronic illness or a disability. Since work and the world are no more dangerous than in the past (in fact, the opposite is true) the rate of disability should not be up. But it is. Our failing system has left people sick, disabled, and unable to work. There are about 6 million more people with a disability in 2023 than in 2008, the first year the government tracked this statistic.[xiv]
Figure 5: US labor force participation rate from 1950[xv]
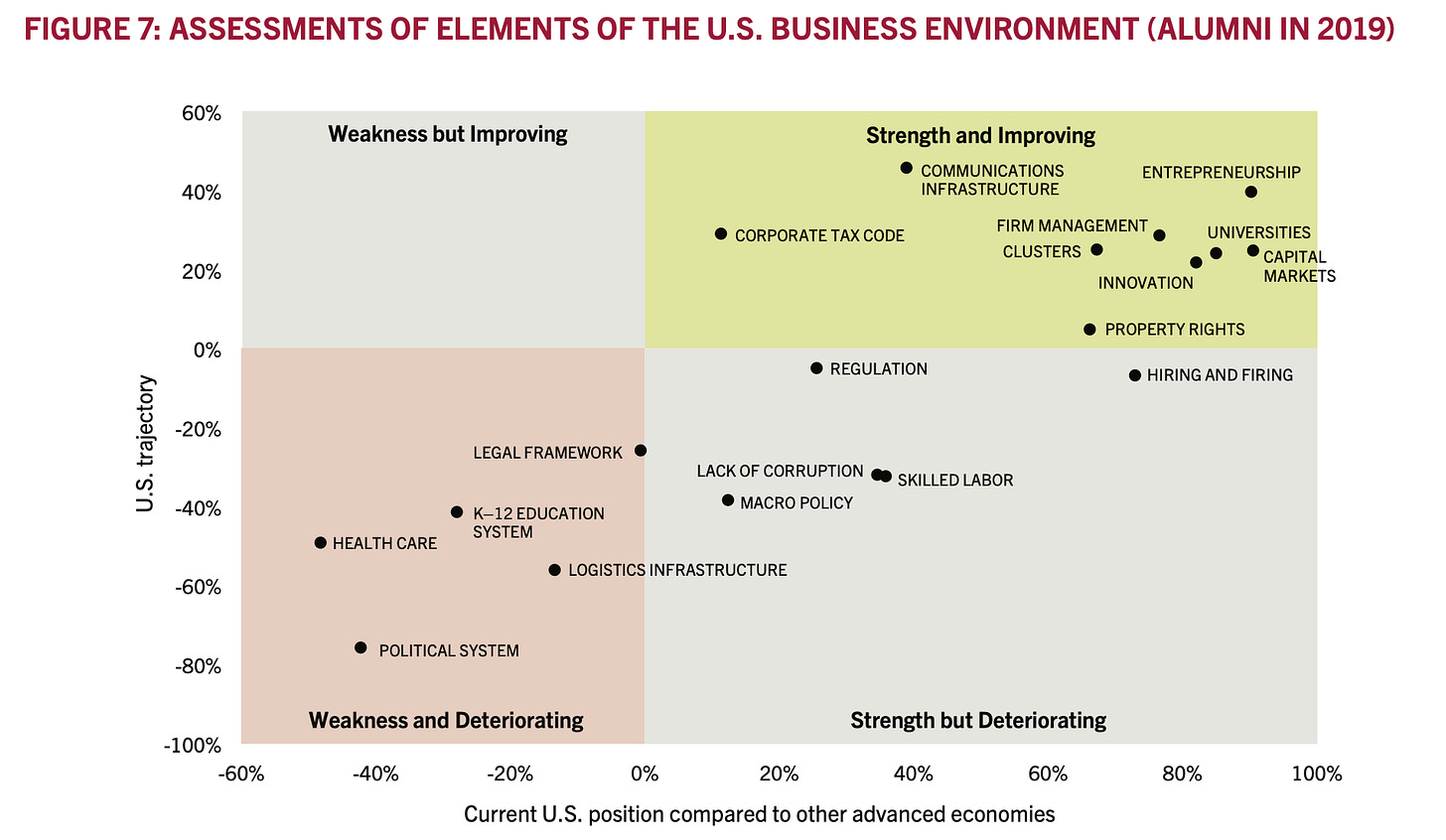
Consequence 4: Declining US Competitiveness
When a global corporation decides where to put its next facility, it can choose from the entire world. It will look at a range of factors including but not limited to the target country’s regulatory regime, political system, and tax code. The corporation will look at the target county’s healthcare system because the health of its workers will determine how productive they are. The US is currently losing this global competition. Harvard Business School periodically surveys its alumni who lead global corporations about aspects of US competitiveness. As Figure 6 shows, the US healthcare system is currently a weakness and deteriorating.
Figure 6: 2019 Harvard Business School US competitiveness survey[xvi]
There is a moral imperative for a rich country to take care of all of its citizens but there is an economic rationale as well. The US healthcare system costs more than other countries and generates worse health outcomes. In short, it is in crisis.
Up Next
In the capstone to the US economy series, Ad Astra will look at the opportunity before us and roll out a plan to restore the American Dream.
[i] https://www.commonwealthfund.org/sites/default/files/2021-08/Schneider_Mirror_Mirror_2021.pdf
[ii] https://www.commonwealthfund.org/sites/default/files/2021-08/Schneider_Mirror_Mirror_2021.pdf
[iii] https://www.reuters.com/article/us-health-lifespan/china-overtakes-u-s-for-healthy-lifespan-who-data-idUSKCN1IV15L
[iv] Our World in Data
[v] https://dianerehm.org/shows/2016-04-12/what-income-and-geography-mean-for-life-expectancy
[vi] https://www.cms.gov/Regulations-and-Guidance/Legislation/EMTALA
[vii] https://newsletters.theatlantic.com/peacefield/61f4c3849d9e380022bdaeb9/big-pharma-tv-drug-ads-legal/
[viii] https://www.salon.com/2023/01/22/with-bigger-tv-advertising-budgets-are-typically-of-low-therapeutic-value-study-says/
[ix] Axios
[x] Keefe, Patrick Radden. Empire of Pain: The Secret History of the Sackler Dynasty. Anchor Books, A Division of Penguin Random House LLC, 2022.
[xi] ChatGPT
[xii] CDC
[xiii] WSJ
[xiv] St. Louis Fed
[xv] St. Louis Fed
[xvi] Harvard Business School